- SPECIALIST ORTHOPAEDIC SURGEON | MELBOURNE, VIC | ALBURY, NSW | MORNINGTON, VIC |
- 03 9421 6133
- Melbourne & Mornington VIC |
- Albury, NSW
Knee arthritis is a common cause of joint pain and stiffness that can gradually limit your ability to walk, stay active, or enjoy everyday life. When these symptoms become more advanced and no longer respond to non-surgical treatments such as physiotherapy, medications, or radio frequency ablation, a total knee replacement surgery may be recommended. This procedure involves replacing the damaged joint surfaces with artificial components to reduce pain and improve movement.
Dr Jason Hockings is an experienced orthopaedic surgeon who uses advanced, patient-specific surgical techniques to restore more natural knee motion and long-term joint function. His approach is tailored to your individual anatomy and lifestyle, with a strong focus on achieving lasting relief and helping you return to the activities that matter most to you.

On this page, you’ll find clear and detailed information about when surgery may be appropriate, the surgical techniques and implants Dr Hockings uses, what to expect during your hospital stay and recovery, potential risks, costs, and frequently asked questions. Whether you’re exploring your options or seeking a second opinion, this guide is designed to help you feel informed and confident about your next steps.
Many people live with knee pain for years, not realising that surgical treatment may be an option. If you’re finding it difficult to walk, stand for long periods, climb stairs, or do the things you enjoy despite trying physiotherapy, medications, or other non-surgical treatments, it may be time to consider whether total knee replacement could help.
Knee problems can gradually chip away at your independence and activity levels. If you’ve noticed a decline in your mobility, or you’re relying more heavily on walking aids or pain medication, it may be worth exploring surgical options.
Dr Jason Hockings will guide you through this decision carefully. He’ll take into account your lifestyle, activity goals, imaging results, and overall health before recommending any procedure. Total knee replacement is not for everyone, but for the right person, it may offer lasting pain relief and a meaningful return to movement.

It’s important to note that outcomes vary depending on factors such as overall health, pre-surgery joint condition, and post-operative rehabilitation. Not every patient will regain full function, but for many, knee replacement may offer a meaningful improvement in quality of life.
Before recommending surgery, Dr Hockings will assess your overall health, joint function, and imaging results. Total knee replacement is not always the first step in treatment, but it may be an appropriate option when symptoms are persistent, progressive, and significantly affect your quality of life.
For people with severe arthritis affecting both knees, Dr Hockings may discuss the option of bilateral knee replacement. This involves replacing both joints during one operation rather than performing two separate procedures months apart.
Bilateral knee replacement may be considered for people who are medically fit, motivated for rehabilitation, and have appropriate support at home. Potential advantages can include a single hospital stay, one anaesthetic, and a combined rehabilitation period. For others, a staged approach may be safer and more practical, particularly when one leg is needed to support early walking and balance.
Recovery after bilateral knee replacement can be more physically demanding in the early stages, which is why careful assessment is essential. Dr Hockings will review your overall health, mobility, home environment, and personal goals to determine whether a simultaneous or staged procedure is the most suitable and safe option for your circumstances.
Choosing to undergo total knee replacement surgery is a major decision. Understanding the surgical techniques available can help you feel more informed and confident in your care. Dr Jason Hockings tailors each procedure to your specific anatomy, goals, and mobility needs, using a combination of well-established and advanced surgical techniques.
This is the most widely used and time-tested approach to knee replacement. During the procedure, the damaged cartilage and bone surfaces of the knee are carefully removed and replaced with prosthetic components designed to mimic natural joint movement. Traditional techniques have a strong track record for improving pain and function, particularly in cases of severe arthritis or joint damage.
Minimally invasive techniques use smaller incisions and aim to reduce trauma to surrounding muscles and soft tissues. For eligible patients, this may result in:
The way your knee is aligned during surgery plays a significant role in how it will feel and function after recovery. Dr Hockings selects the most suitable alignment method based on your individual knee anatomy:
This traditional approach aims to create a straight line from the hip to the ankle, ensuring even weight distribution across the implant. It can enhance joint stability and reduce the risk of early wear.
Kinematic alignment aims to restore your natural, pre-arthritic joint position by aligning the implant to match the original curves and angles of your knee. This more personalised method may improve comfort, motion, and the “natural feel” of your new joint.
Instead of cutting through the quadriceps tendon, this muscle-sparing technique accesses the joint by gently moving the muscles aside.
This may allow for:
Using detailed 3D images from your pre-operative CT scan, custom cutting guides are created specifically for your anatomy.
This supports:
Dr Hockings uses augmented reality (AR) technology to visualise the joint in real time during surgery.
This system allows for:
In selected cases, robotic technology may be used to assist with bone preparation and implant alignment. While not necessary for every case, robotics can offer added accuracy in certain anatomical situations or revision procedures.
During total knee replacement surgery, damaged joint surfaces are removed and replaced with artificial components designed to replicate the natural function of your knee. Dr Jason Hockings uses advanced implant designs and materials that aim to provide long-lasting durability, stability, and comfort tailored to your unique anatomy and activity level.
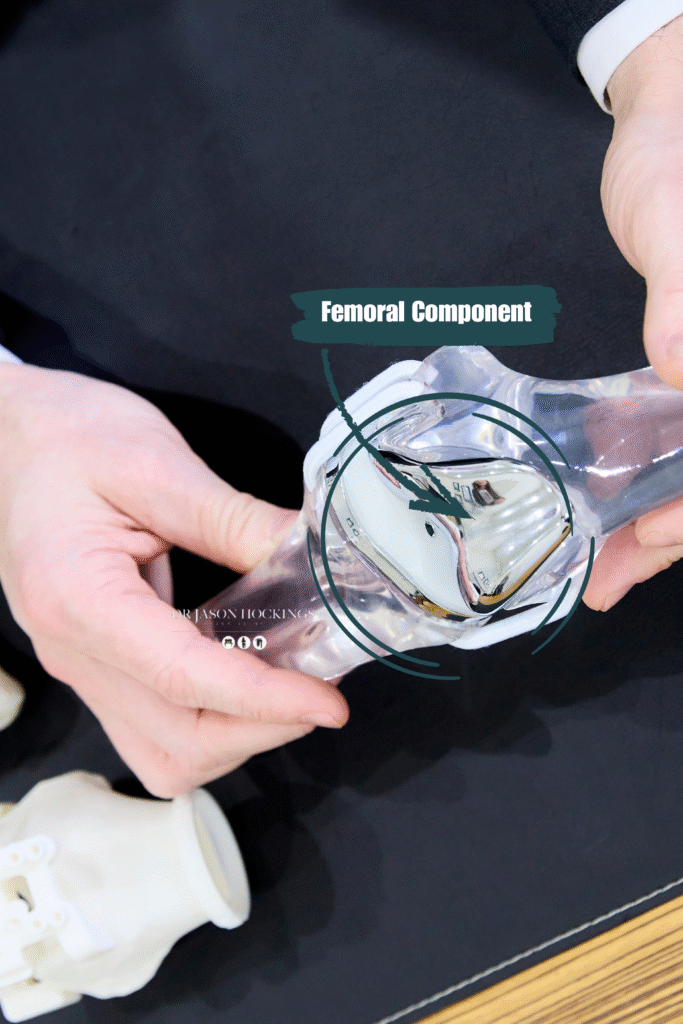
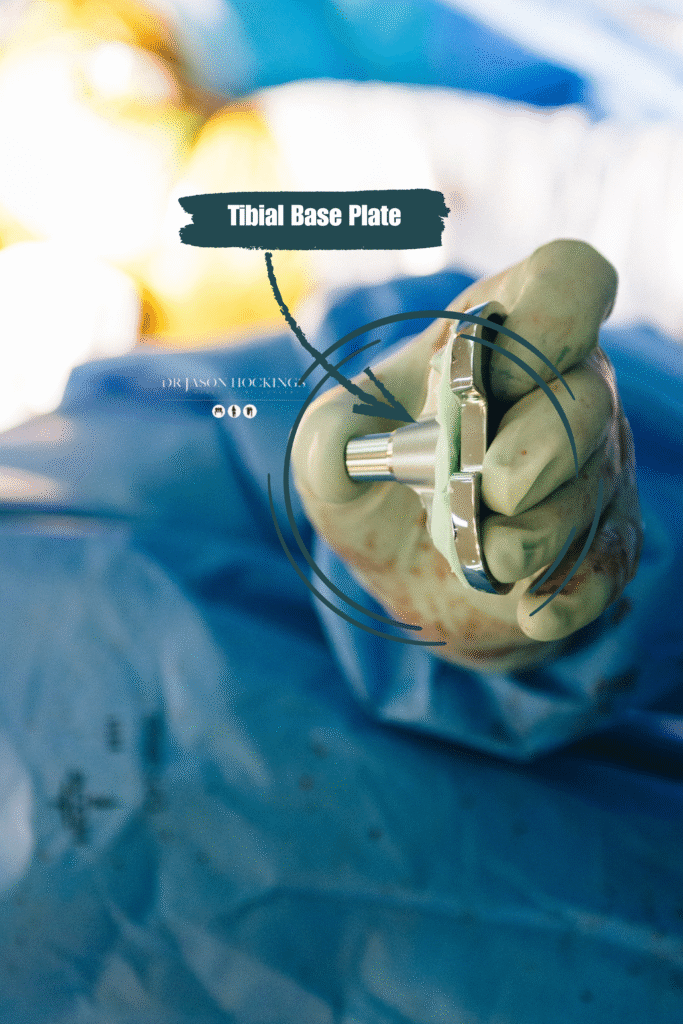
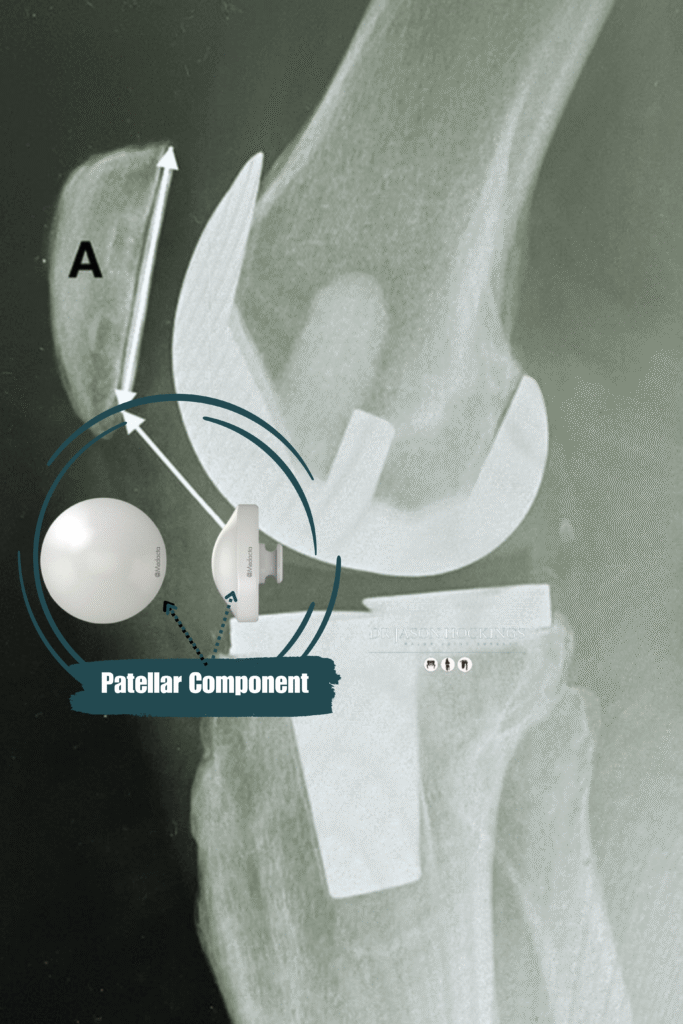
Prosthetic Components
A total knee replacement typically involves three main components:
A metal cap that covers the end of the thigh bone (femur). This part is shaped to allow smooth bending and flexing of the knee.
A metal baseplate that sits on the top of the shin bone (tibia), often with a polyethylene (plastic) insert that serves as the new weight-bearing surface.
A plastic button that may be attached to the underside of the kneecap (patella), depending on the degree of wear and the condition of your natural cartilage.
IMPLANT MATERIALS & DESIGN
Dr Hockings primarily uses a medial pivot implant, (GMKSphere). This design differs from traditional implants by mimicking the knee’s natural movement more closely. The medial pivot allows the inner (medial) side of the knee to act as a stable pivot point, while the outer (lateral) side moves more freely, similar to how a healthy knee works.
All materials used are carefully selected to reduce the risk of allergic reaction, corrosion, or mechanical failure.
IMPLANT FIXATION METHODS
Dr Hockings most commonly uses cementless (press-fit) fixation, where the implant is designed to encourage natural bone growth into the surface of the component. This biological fixation method may offer long-term durability and is well-suited to patients with good bone quality. In some cases, cemented fixation may be used, especially if bone quality is lower or if other clinical factors suggest it would be more appropriate. Cemented implants are bonded to the bone using a special surgical cement, allowing immediate fixation.
The choice of implant design, materials, and fixation method is made following a detailed evaluation of your knee anatomy, lifestyle, activity level, and bone quality. During pre-operative planning, Dr Hockings uses 3D imaging and patient-specific instrumentation (PSI) to determine the most appropriate components for your individual needs. This customised approach helps ensure that your knee replacement not only fits well and functions naturally but also supports a smooth and confident return to your daily life.
If you and Dr Jason Hockings decide that total knee replacement surgery is the right path for you, it’s natural to wonder what the journey will involve. This step-by-step guide explains exactly what to expect from your first appointment, through surgery, and into recovery using Dr Hockings’ advanced, patient-specific, kinematically aligned approach.
Step 1
 Your journey begins with a referral from your GP or another medical specialist. This is required to book your first appointment with Dr Hockings and ensures you receive the appropriate Medicare rebate.
Your journey begins with a referral from your GP or another medical specialist. This is required to book your first appointment with Dr Hockings and ensures you receive the appropriate Medicare rebate.
During your initial consultation, Dr Hockings will:
If total knee replacement is recommended, Dr Hockings will review the procedure with you, including the risks, benefits, and expected recovery. Once you’re confident and informed, you’ll sign a consent form. You’ll also receive advice on preparing your home and organising any support you may need after surgery.
Step 2
 After your initial consultation, you’ll receive a referral for a CT scan of your entire leg, from hip to ankle. This detailed scan captures the precise structure of your bones and joints and is used to create a highly accurate 3D digital model of your knee.
After your initial consultation, you’ll receive a referral for a CT scan of your entire leg, from hip to ankle. This detailed scan captures the precise structure of your bones and joints and is used to create a highly accurate 3D digital model of your knee.
This 3D model becomes the foundation for your personalised surgical plan, and with the support of advanced software, Dr Hockings can, prior to your surgery:
Once Dr Hockings has finalised the plan, the data is securely transferred to a specialist manufacturing facility in Switzerland, where your patient-specific instruments (PSI) are created. These 3D-printed surgical cutting guides are designed to fit your knee precisely, then sterilised and delivered to the hospital in time for your operation.
Step 3
 In the weeks leading up to surgery, you’ll receive support from Dr Hockings’ team to prepare, including:
In the weeks leading up to surgery, you’ll receive support from Dr Hockings’ team to prepare, including:
Step 4
 Before your procedure, you’ll have a pre-operative consultation with the anaesthetic team, usually conducted over the phone. During this conversation, the anaesthetist will review your medical history, current medications, and any previous experiences with anaesthesia. This is an important step in ensuring your safety and comfort during surgery. Together, you’ll discuss the two main types of anaesthesia used in knee replacement surgery; spinal anaesthesia and general anaesthesia and determine which is most appropriate for you:
Before your procedure, you’ll have a pre-operative consultation with the anaesthetic team, usually conducted over the phone. During this conversation, the anaesthetist will review your medical history, current medications, and any previous experiences with anaesthesia. This is an important step in ensuring your safety and comfort during surgery. Together, you’ll discuss the two main types of anaesthesia used in knee replacement surgery; spinal anaesthesia and general anaesthesia and determine which is most appropriate for you:
The anaesthetist will explain the risks and benefits of each option and answer any questions you may have. Their goal is to create a personalised anaesthetic plan that prioritises your comfort, supports a smooth surgical experience, and promotes a safe recovery.
Step 5.
 Your total knee replacement procedure is a carefully planned and highly technical operation designed to relieve pain, improve movement, and restore confidence in your daily activities. Here’s what to expect during the surgery itself.
Your total knee replacement procedure is a carefully planned and highly technical operation designed to relieve pain, improve movement, and restore confidence in your daily activities. Here’s what to expect during the surgery itself.
Anaesthesia and surgical preparation
On arrival at the operating theatre, you will be greeted by the anaesthetic team. Your anaesthetist will review your medical history and ensure that your chosen anaesthesia method is safely administered. .
Once anaesthesia takes effect, your surgical leg will be carefully positioned to optimise access and precision. The skin will be cleaned thoroughly with an antiseptic solution to reduce the risk of infection, and sterile drapes will be applied to maintain a clean surgical field.
Surgical incision using the Subvastus Approach
Dr Hockings performs most knee replacements using the Subvastus Approach. Unlike traditional techniques that cut through the quadriceps tendon, the subvastus approach gently lifts the muscle to access the joint beneath it. This minimally invasive, muscle-sparing technique offers several potential benefits:
An incision is made along the front of your knee, carefully sized and positioned to allow optimal access to the joint while preserving surrounding tissues.
Exposure and assessment of the joint
With the knee joint now exposed, Dr Hockings will assess the extent of joint damage and confirm key measurements. He examines the worn cartilage, checks bone surfaces, and confirms the alignment and motion of the joint. At this stage, Patient-Specific Instrumentation (PSI) the custom-made cutting guides created from your CT scan are positioned on the femur (thigh bone) and tibia (shin bone). These guides allow precise bone cuts that match your 3D surgical plan and intended kinematic alignment.
Specialised callipers and measuring devices may also be used to:
This step is critical to achieving a well-balanced, anatomically accurate reconstruction of your knee.
Bone preparation and use of MyKnee PSI
Using the MyKnee PSI guides, Dr Hockings removes the damaged bone and cartilage surfaces in a way that matches your unique anatomy. This allows:
The goal is to restore the natural movement and feeling of your knee, using a kinematically aligned approach rather than forcing the joint into a generic position.
Trial implants and soft tissue balancing
Before the final implants are inserted, trial components are placed onto the prepared bone surfaces. These temporary pieces allow Dr Hockings to assess:
If adjustments are needed, they are made at this stage to ensure the final implants provide a smooth, stable, and functional result.
Insertion of the final implants
Once satisfied with the balance and alignment, Dr Hockings will implant the final components:
Dr Hockings predominantly uses cementless (press-fit) fixation techniques, which are designed to allow your natural bone to grow into the surface of the implants over time. This approach is often preferred in patients with good bone quality and may offer advantages in long-term durability and biological integration. In certain cases, such as patients with softer bone or revision surgery, bone cement may be used to help secure one or more components. The choice of fixation method is based on your individual anatomy, bone strength, and overall surgical plan.
Advanced surgical technology, such as Augmented Reality (NextAR) or Robotic-Assisted techniques, may also be used in select cases. These tools enhance real-time visualisation and accuracy during implant positioning, supporting precise alignment and potentially improving long-term outcomes. Dr Hockings will determine whether these technologies are appropriate for your specific case during the planning phase.
Closing the incision
Once the final implants are secured and joint function is confirmed, the surgical area is irrigated and checked for stability. The incision is then closed in layers:
You’ll then be transferred to the recovery unit, where your vital signs will be monitored and your post-operative journey will begin.
Step 6.
 Once your surgery is complete, you’ll be monitored in a recovery area while the effects of anaesthesia wear off. You may experience some pain or swelling, but this will be carefully managed using medications and other strategies to keep you as comfortable as possible.
Once your surgery is complete, you’ll be monitored in a recovery area while the effects of anaesthesia wear off. You may experience some pain or swelling, but this will be carefully managed using medications and other strategies to keep you as comfortable as possible.
Getting out of bed and walking, with assistance, usually begins within 24 hours of surgery as moving early helps reduce the risk of complications such as blood clots and stiffness. You’ll be encouraged to wear your own clothes soon after surgery, an important step in regaining mobility and confidence.
Most patients stay in hospital for 1 to 3 days following surgery. During this time, you’ll begin the early phases of recovery with close support from your surgical and physiotherapy team.
What to expect in hospital:
Before you leave hospital, Dr Hockings’ team will ensure you’re ready for the next phase of recovery. You’ll be given personalised instructions and support, including:
This is a critical period for healing and regaining independence. It’s normal to feel tired and experience discomfort, but with steady progress, your confidence will grow.
Key milestones:
This phase focuses on restoring joint flexibility and improving the strength of muscles that support your knee.
Your physiotherapy goals:
Some patients may be cleared to return to driving or return to work, especially if your job is desk-based at around week 4 to 6, depending on your progress and which leg was operated on.
By this stage, your mobility should be improving significantly, and you may start feeling more confident moving around your home and community.
What to expect:
This is the point where many patients begin to experience the full benefits of surgery, improved movement, reduced pain, and increased participation in everyday life.
Milestones to expect:
While you may feel “recovered” earlier, complete healing from total knee replacement often takes up to 12 months. By this time, most patients have minimal pain, good range of motion, and a stable, strong joint.
Ongoing care:
With a well-supported recovery plan and your active participation in rehabilitation, you’ll be on track to regain freedom of movement and achieve long-lasting benefits from your knee replacement. Dr Hockings and his team are here to support your journey, every step of the way.
While total knee replacement is a common and generally safe procedure, like all surgeries, it carries certain risks. Understanding these risks can help you make an informed decision and recognise any signs that may require further attention during your recovery. Dr Hockings will discuss these potential risks with you during your consultation and take every precaution to minimise them.
Some patients may experience persistent pain, limited range of motion, or stiffness despite a successful procedure. Rehabilitation is key to reducing these risks.
Some risks are common to many types of orthopaedic surgery and are generally low, especially when performed by experienced surgeons in well-equipped hospitals:
Dr Jason Hockings takes a highly individualised and technology-enhanced approach to knee replacement surgery, with a strong focus on reducing complications and supporting a safe, effective recovery. Several key strategies are used throughout your care journey to help minimise risk:
Using 3D imaging and CT-based planning, Dr Hockings uses custom-made surgical guides tailored to your unique anatomy. These guides support greater precision and consistency during surgery, which may help reduce complications and improve implant positioning.

Dr Hockings typically uses the subvastus approach, which spares the quadriceps tendon by accessing the knee joint beneath the muscle. This technique helps preserve muscle strength, reduce pain, and promote faster early mobility.
To reduce the risk of infection and improve surgical workflow, Dr Hockings uses high-quality single-use disposable instruments. These pre-sterilised, individually packaged tools ensure cleanliness and consistency, while avoiding issues related to reprocessing reusable equipment.

Together, these steps reflect Dr Hockings’ commitment to patient safety, surgical accuracy, and high-quality care, helping to ensure the best possible outcome from your knee replacement surgery.
Every surgery carries risk, but the majority of patients undergoing total knee replacement experience significant improvements in mobility, pain reduction, and overall quality of life. Dr Hockings and his team are committed to guiding you through every stage of the process, with careful planning and expert care to reduce complications and support a smooth recovery.
The cost of total knee replacement surgery in Australia depends on several factors, including whether you hold private health insurance, are self-funding, or are accessing care through the public system. Below is a summary of what you can expect in each setting.
If you’re referred through the public system, your surgery and hospital stay are fully covered by Medicare, with no out-of-pocket cost. There may, however, still be some costs associated with pre- and post-operative care provided outside the hospital.
Public system process:
Additional costs to consider: While the surgery itself is covered, you may still need to pay for:
If you have private health insurance, you may be eligible to have your total knee replacement surgery performed by Dr Jason Hockings in a private hospital setting, with significantly reduced wait times and the ability to choose your surgeon.
What does your private hospital insurance cover?
Most of your hospital, theatre fees & implants will typically be covered by your insurer, provided your policy includes joint replacement and you have served any applicable waiting periods.
Your level of cover matters:
To be covered for joint replacement surgery, Silver Hospital Cover or higher is generally required. Most Silver, Silver Plus, and Gold policies include joint replacement under their list of covered procedures.
Out-of-pocket costs
While the hospital stay may be mostly covered by your insurer, there may still be gap payments (out-of-pocket costs) for:
Surgeons across Australia are free to set their own fees, which can vary widely. Dr Hockings chooses to align his fees with the Australian Medical Association (AMA) schedule, a nationally recognised guide to fair medical fees that adjusts for inflation. For a typical total knee replacement, the out-of-pocket (gap) fee for surgery with Dr Hockings is usually just over $3,000. This represents excellent value compared to many other surgeons, who may charge $5,000 or more for similar procedures.
Dr Hockings is committed to making high-quality orthopaedic care accessible and transparently priced. His clear, upfront cost structure ensures you understand what to expect, with no hidden fees or surprises.
If you don’t have private health insurance, you can still choose to have your knee replacement surgery with Dr Hockings as a self-funded patient. Many patients who are not privately insured choose to self-fund surgery with Dr Hockings to avoid extended delays in the public system. This option allows you to receive timely care from a highly trained surgeon in a private hospital setting, without needing private health cover.
Total cost range: $25,000 – $35,000 AUD (all-inclusive).
This includes:
Additional costs to consider:
Dr Hockings’ team will help guide you through the financial process and provide a personalised cost breakdown based on your situation. If you’re unsure whether your private health fund covers joint replacement surgery, we encourage you to contact your insurer before your consultation. Transparent information and support will be provided every step of the way so you can feel informed and confident in making financial decisions related to your care.
Dr Jason Hockings is a highly qualified orthopaedic surgeon with extensive experience in treating knee arthritis and performing advanced knee replacement procedures using evidence-based, modern techniques.
Dr Hockings uses cutting-edge surgical planning technology, including 3D CT-based mapping and Patient-Specific Instrumentation (PSI), to perform kinematically aligned total knee replacements. This personalised technique aims to replicate your natural joint motion and biomechanics, which may support a more natural-feeling knee and improved function.
Where appropriate, Dr Hockings uses a muscle-sparing surgical technique that avoids cutting the quadriceps tendon. This subvastus approach is designed to preserve strength and may assist with a smoother, faster recovery.
For select cases, Dr Hockings incorporates innovative tools such as Augmented Reality (NextAR) and Robotic-Assisted techniques to improve surgical accuracy and support optimal implant positioning.
You’ll receive clear explanations, thorough preparation, and compassionate support at every stage of your journey, from your first consultation to your final recovery milestone.
Dr Hockings is dedicated to helping you return to the activities you enjoy with less pain and greater confidence. He focuses not just on the surgical procedure, but on your long-term mobility, function, and satisfaction.
If you’re experiencing persistent knee pain, stiffness, swelling, or difficulty walking that hasn’t improved with physiotherapy, medications, or injections, you may be a candidate for knee replacement surgery. A referral to Dr Hockings from your GP can help begin the assessment process.
Kinematic alignment is a technique that aims to restore your knee to its original, pre-arthritic alignment and motion, rather than forcing it into a standard mechanical position. This approach may improve how natural the new joint feels and functions.
PSI involves creating custom-made 3D-printed surgical guides based on a CT scan of your leg. These guides are designed to match your unique knee anatomy and are used during surgery to help position the implants with high precision.
You’ll usually begin walking (with assistance) on the same day or the morning after surgery. Walking aids such as crutches or a frame are used initially and gradually phased out as your strength and balance improve.
All surgery carries some risk. Potential complications include infection, blood clots, stiffness, or prosthesis-related issues. Dr Hockings will explain the risks in detail and take steps to minimise them as part of your surgical planning.
These techniques access the knee by gently lifting the muscles rather than cutting through them. By preserving the surrounding soft tissues, the approach may support more comfortable early movement and a smoother transition into rehabilitation.
NextAR uses real-time digital overlays to guide implant alignment during surgery. This technology supports accurate positioning based on your personalised plan while maintaining a streamlined and minimally invasive workflow.
Robotic technology provides real-time guidance and controlled bone preparation during surgery. It works with your pre-operative plan to support accurate implant placement tailored to your individual anatomy.
Kinematic alignment focuses on restoring your knee’s natural pre-arthritic motion and joint angles. This approach aims to position the implant in a way that reflects your individual anatomy, helping the knee move in a pattern that feels more familiar and balanced.
Medial pivot implants are designed to mimic the natural rolling and gliding pattern of a healthy knee. This design provides a stable pivot point on the inner side of the joint, which may help the knee feel more controlled during everyday movement.
PSI uses custom 3D-printed guides created from your CT scan to assist with precise bone preparation during surgery. This approach supports accurate implant positioning tailored to your individual anatomy and pre-operative surgical plan.

If you’re experiencing ongoing pain, stiffness, or reduced movement that is affecting your daily activities or quality of life, a thorough orthopaedic assessment can help determine the cause and guide the most appropriate treatment options for your situation.