- SPECIALIST ORTHOPAEDIC SURGEON | MELBOURNE, VIC | ALBURY, NSW | MORNINGTON, VIC |
- 03 9421 6133
- Melbourne & Mornington VIC |
- Albury, NSW
Shoulder impingement and subacromial bursitis are common sources of pain, particularly when lifting the arm or performing overhead movements. These conditions often occur together and can lead to inflammation, discomfort, and reduced shoulder function. Shoulder impingement refers to the pinching of soft tissues, such as the rotator cuff tendons or bursa, between the upper arm bone (humerus) and the bony arch of the shoulder (acromion). Over time, this repeated compression may lead to bursitis, which is inflammation of the small fluid-filled sac (bursa) that helps cushion and reduce friction in the joint.

Shoulder impingement and bursitis are common causes of pain in the upper arm and shoulder, particularly during overhead movement. Both conditions involve irritation of the soft tissues within the subacromial space, the narrow area between the top of the upper arm bone (humerus) and the overlying bony arch of the shoulder (acromion).
Shoulder impingement occurs when the rotator cuff tendons become pinched or compressed during arm elevation. This repeated friction can lead to inflammation and pain.
Subacromial bursitis refers to inflammation of the bursa, a small fluid-filled sac that cushions the tendons and reduces friction within the shoulder. These conditions frequently occur together and may also be associated with rotator cuff pathology.
Dr Jason Hockings will begin with a thorough clinical examination of your shoulder, reviewing your symptoms, range of motion, and rotator cuff strength.
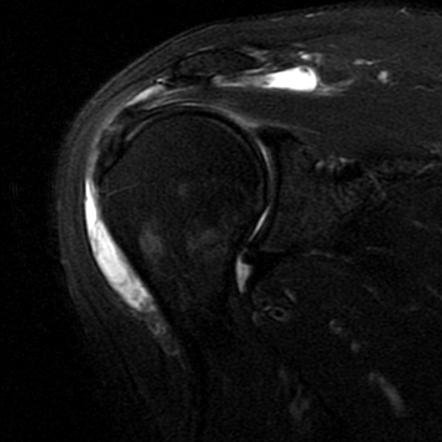
Imaging such as X-rays may be used to check for bone spurs or structural narrowing. Ultrasound or MRI can help confirm inflammation of the bursa, detect fluid buildup, and identify any coexisting rotator cuff tears.
A diagnostic injection of local anaesthetic into the subacromial space may also be used — temporary pain relief following the injection supports the diagnosis of impingement or bursitis.
Surgery may be considered if your symptoms persist despite a full course of non-operative management, or if imaging reveals structural narrowing, rotator cuff damage, or significant mechanical impingement that is unlikely to resolve with physiotherapy alone.
Dr Hockings will discuss the role of surgery only after careful consideration of your condition, lifestyle, goals, and response to conservative treatment.
If non-surgical options are not effective, arthroscopic subacromial decompression may be recommended. This is a minimally invasive (keyhole) procedure performed under general anaesthetic. Using a small camera (arthroscope) and specialised instruments inserted through tiny incisions, Dr Hockings removes inflamed tissue from the bursa and smooths the underside of the acromion bone. This creates more space for the rotator cuff to move freely, reducing mechanical friction and inflammation.
The surgery is usually performed as a day procedure, and recovery is generally quicker than with rotator cuff repair. Many patients resume light activities within a few weeks, with full recovery taking several months depending on your rehabilitation progress.

If you’re experiencing ongoing pain, stiffness, or reduced movement that is affecting your daily activities or quality of life, a thorough orthopaedic assessment can help determine the cause and guide the most appropriate treatment options for your situation.