- SPECIALIST ORTHOPAEDIC SURGEON | MELBOURNE, VIC | ALBURY, NSW | MORNINGTON, VIC |
- 03 9421 6133
- Melbourne & Mornington VIC |
- Albury, NSW
If you’ve previously had a knee replacement but are now experiencing pain, stiffness, instability, or other complications, revision knee replacement surgery may be necessary to restore joint function and improve your quality of life. This page explains what revision knee replacement involves, why some knee replacements may become painful or fail over time, and what you can expect from the assessment, surgery, and recovery process. You’ll also learn about the signs that may indicate a problem with your current implant, the surgical options available, and how Dr Jason Hockings approaches complex revision procedures with precision and personalised care.

Radiofrequency ablation (RFA) works by disrupting the sensory nerve pathways that transmit pain signals from the knee joint to the brain. The procedure specifically targets the genicular nerves, which are responsible for carrying pain messages from within the knee. Because these nerves are the focus of treatment, the procedure is also known as genicular nerve ablation.
In individuals with knee osteoarthritis, these sensory nerves can become overactive due to ongoing inflammation, cartilage wear, and changes in joint mechanics. This can result in persistent, hard-to-manage pain, even after trying physiotherapy, medications, or injections.
During the procedure, Dr Hockings uses real-time imaging (typically X-ray or ultrasound) to guide the placement of a thin, needle-like probe near the genicular nerves. Once accurately positioned, the tip of the probe delivers a controlled dose of radiofrequency energy, which generates heat to create a small lesion on the nerve. This temporarily interrupts the nerve’s ability to transmit pain signals.
Importantly, RFA does not change the structure of the joint itself. Instead, it helps reduce pain perception, allowing for improved mobility, greater comfort, and the ability to participate more easily in daily activities, all without the need for incisions, stitches, or surgical recovery.

Most knee replacements provide many years of pain relief and improved mobility however, in some cases, a knee replacement may become painful, unstable, or worn over time. When this happens, revision knee replacement surgery may be recommended.
Revision knee replacement is a specialised procedure that involves removing part or all of the original knee implant and replacing it with new components. Depending on the condition of the joint and surrounding bone, the surgery may also involve rebuilding damaged bone with grafts, using metal augments, or implanting more stabilised prostheses.
Unlike a first-time (primary) knee replacement, revision surgery is more complex. It may take longer to perform, and the recovery process can be more involved. The goal is to restore function, improve stability, and reduce pain, particularly when symptoms from a failing implant begin to affect your daily activities and quality of life.
Dr Jason Hockings has a special interest in managing complex knee conditions, including revision procedures. If your previous knee replacement has not met expectations, he can conduct a thorough assessment to determine whether revision surgery may be appropriate and provide a clear treatment plan based on your individual situation.

Revision knee replacement surgery is typically considered when the original (primary) knee replacement is no longer functioning effectively or is causing significant pain, instability, or limitation in mobility. Not all knee pain after joint replacement is caused by implant failure however, as there may be other treatable causes such as inflammation, scar tissue, referred pain from the hip or spine, or soft tissue irritation.
Dr Hockings will only recommend revision surgery when non-operative options are no longer appropriate, and when imaging or testing confirms that the implant is contributing to your symptoms. His approach is tailored to your individual needs and guided by a careful review of the risks, expected outcomes, and your overall health status.
Revision knee replacement surgery often involves more than simply exchanging old components for new ones. Over time, changes in bone quality, soft tissues, or ligament support may make standard implants inadequate. Modern revision implant systems are specially designed to address these complexities, offering improved support, alignment correction, and durability.
Whereas a primary knee replacement typically uses standard-sized components, revision implants come in a broader range of configurations to account for bone loss, ligament damage, or joint instability. Dr Hockings uses advanced revision implant systems tailored to your anatomy, surgical history, and functional needs.
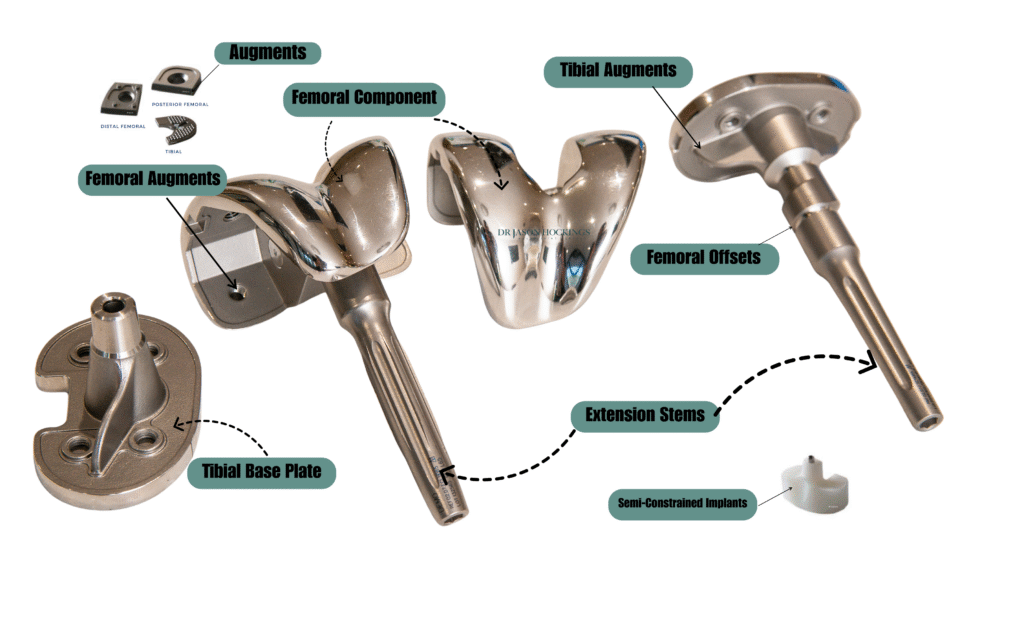
Dr Hockings is experienced in selecting and positioning these components based on detailed imaging and preoperative planning. Every revision case is different, and his tailored approach ensures that the most appropriate combination of implants is used to restore comfort, stability, and joint function as effectively as possible.
Step 1
Before proceeding with revision surgery, it’s crucial to determine the underlying cause of your symptoms and assess your overall health.
Key investigations may include:
You will also be assessed by a general medical specialist to ensure you are medically fit for surgery. This allows time to manage any other health issues that may increase the risk of complications. Your anaesthetist will discuss the best anaesthesia approach and postoperative pain relief options tailored to your needs.
Step 2
If your revision surgery is not related to infection, the procedure is typically performed in a single stage:
Step 3
If infection is present, a two-stage revision is recommended.
Stage One: Infection control
Stage Two: Definitive implant placement
Step 4
Step 5
Recovery after revision knee replacement is generally longer than a primary knee replacement. Dr Hockings provides a structured follow-up schedule to track your healing:
2 weeks
8 weeks
4 months
12 months
While many patients return to walking, driving, and low-impact activities within a few months, complete recovery can take longer than a primary knee replacement, often up to 6 to 12 months. Some limitations on high-impact sports or repetitive movements may remain, depending on the structural changes made during revision.
Revision knee replacement is a major operation, but with appropriate planning, support, and rehabilitation, it may offer significant improvements in stability, pain relief, and quality of life.

Revision knee replacement is among the most complex procedures in orthopaedic surgery. It requires a detailed understanding of why a previous knee replacement may have failed, how joint mechanics have changed over time, and what surgical techniques can best restore comfort and mobility.
Dr Jason Hockings is an experienced orthopaedic surgeon who manages both primary and revision knee replacements. He has extensive experience treating patients with challenging knee problems, including implant loosening, joint instability, infection, and bone loss.
Each revision case is carefully assessed using advanced imaging and digital planning tools to understand the underlying cause and determine the most appropriate treatment strategy. Dr Hockings selects from a range of implant systems, augments, and bone reconstruction techniques to match the specific needs of each individual patient and care is coordinated across a multidisciplinary team that includes anaesthetists, physicians, physiotherapists, and nursing staff.
From your initial assessment through to your recovery, the goal is to provide well-considered, individualised care that supports a safe procedure and a steady return to movement and daily life.

If you’re experiencing ongoing pain, stiffness, or reduced movement that is affecting your daily activities or quality of life, a thorough orthopaedic assessment can help determine the cause and guide the most appropriate treatment options for your situation.