- SPECIALIST ORTHOPAEDIC SURGEON | MELBOURNE, VIC | ALBURY, NSW | MORNINGTON, VIC |
- 03 9421 6133
- Melbourne & Mornington VIC |
- Albury, NSW
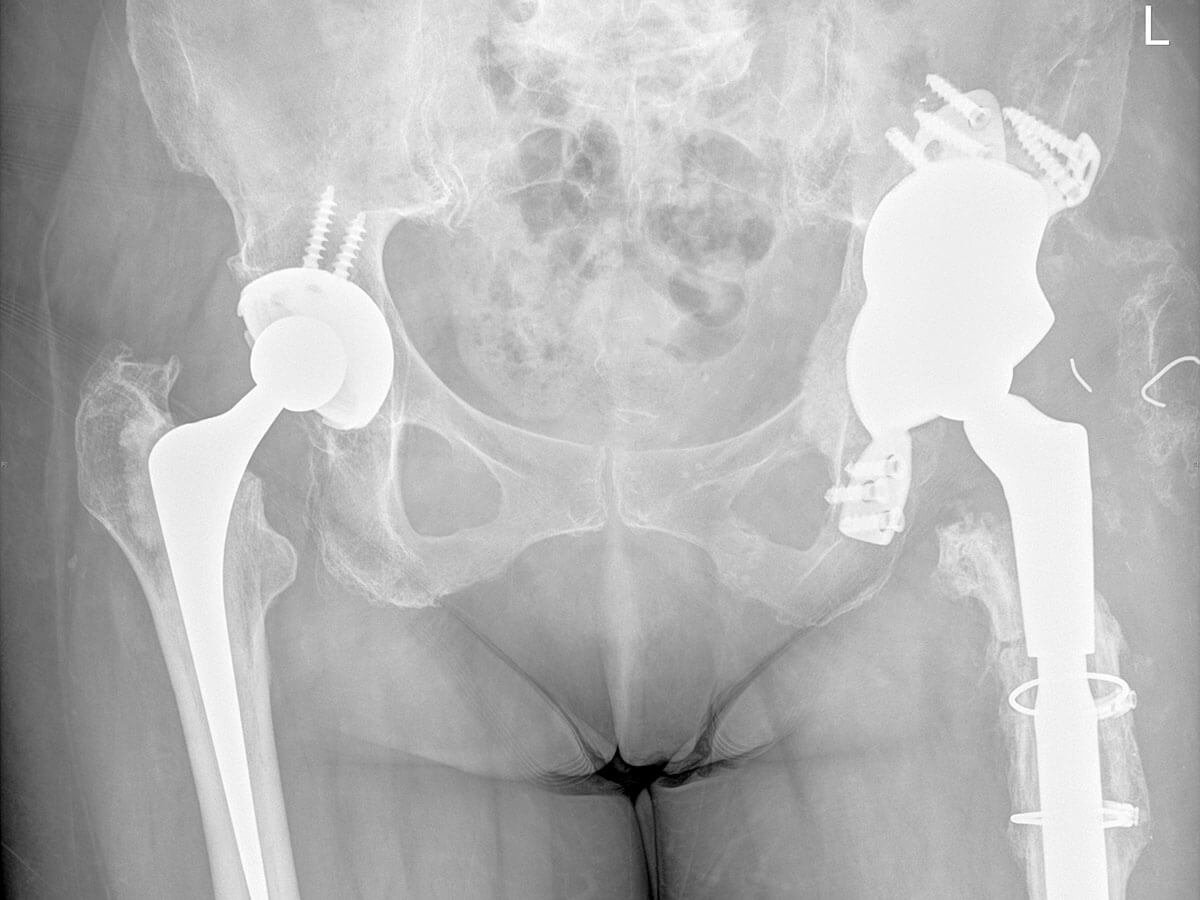
Revision hip replacement surgery, also known as revision hip arthroplasty, is a complex procedure performed to address problems that can develop after a previous hip replacement. This may include pain, implant loosening, infection, dislocation, or wear of the prosthetic components. This page provides a detailed guide to help you understand what revision surgery involves, why it may be recommended, and what to expect before, during, and after the procedure. It is designed to equip you with clear, practical information and support as you prepare for surgery with Dr Jason Hockings.

Occasionally, a primary hip replacement may require revision due to persistent pain, implant wear, instability, loosening, fracture, or infection. Revision hip replacement surgery involves the careful removal and replacement of one or more components of the original hip prosthesis.
Depending on your individual condition, this procedure may also require the reconstruction of bone or soft tissue using bone grafts, augments, or specialised revision implants designed to restore stability and function. In cases of infection, a staged approach may be necessary, involving temporary spacers and antibiotic treatment before reimplantation.
Revision hip replacement is technically more complex than a primary procedure, requiring advanced surgical planning, careful handling of bone and soft tissues, and the use of specialised implants. Dr Jason Hockings has extensive experience in revision hip arthroplasty and will tailor your surgical plan to address your unique anatomy, diagnosis, and previous surgical history.
In many cases, problems with a hip implant develop gradually. Recognising the warning signs of a failing hip replacement early can lead to timely intervention and help prevent further complications. If you experience any of the following symptoms, it’s important to arrange a review with Dr Jason Hockings for a thorough evaluation.

If a deep infection is present, a two-stage approach is often recommended. In the first stage, the prosthesis is removed, and a temporary antibiotic-loaded spacer is inserted. After the infection is cleared (typically over several weeks to months), a second operation is performed to implant a new hip replacement.
Revision hip replacement surgery requires a carefully planned and highly individualised approach. Unlike a primary hip replacement, which often follows a standardised pathway, revision procedures are more complex and must be tailored to address the unique issues associated with your existing implant, bone structure, and soft tissues. Dr Jason Hockings draws on advanced diagnostic tools, surgical experience, and evidence-based techniques to formulate a surgical plan that prioritises stability, longevity, and function.
Revision hip surgery typically takes longer than a standard hip replacement, anywhere from 2 to 4 hours depending on the complexity of the case and whether reconstruction is required. You will be monitored in recovery before returning to the ward.


There are several things you can do before and after surgery to reduce your risk of complications:
If you’re experiencing problems with your existing hip replacement, you’re not alone and you’re not without options. Revision hip replacement surgery is a specialised procedure that requires careful planning, clinical experience, and a personalised approach to ensure the best possible outcome.
Dr Jason Hockings is a fellowship-trained orthopaedic surgeon with extensive experience in complex primary and revision hip arthroplasty. He uses a methodical, patient-centred approach supported by the latest imaging, planning software, and surgical techniques to deliver safe and effective care.
Your care doesn’t end in the operating theatre. Dr Hockings is committed to supporting you throughout your recovery, with scheduled follow-up appointments, coordinated physiotherapy, and ongoing education to help you regain confidence and mobility.
Patients often report significant improvements in pain relief, stability, and function following revision hip replacement, especially when they are well-prepared and actively involved in their recovery process.
If you’re concerned about a painful or failing hip replacement, Dr Jason Hockings can provide clarity and expert guidance. A personalised consultation will help determine whether revision surgery is right for you, and what steps to take next.
If you’re experiencing ongoing pain, stiffness, or reduced movement that is affecting your daily activities or quality of life, a thorough orthopaedic assessment can help determine the cause and guide the most appropriate treatment options for your situation.