- SPECIALIST ORTHOPAEDIC SURGEON | MELBOURNE, VIC | ALBURY, NSW | MORNINGTON, VIC |
- 03 9421 6133
- Melbourne & Mornington VIC |
- Albury, NSW
Reverse shoulder replacement, also known as reverse total shoulder arthroplasty (RTSA) is a specialised type of joint replacement surgery used to treat complex shoulder conditions. It is most commonly recommended when there is severe or irreparable rotator cuff damage, rotator cuff arthropathy (a combination of arthritis and cuff tearing), or a previously failed shoulder surgery.
The procedure is called a “reverse” because it changes the position of the joint components: the ball-shaped implant is placed where the shoulder socket (glenoid) once was, and the socket is positioned where the humeral head used to be. This reversed design shifts the mechanics of the shoulder, allowing the deltoid muscle to take over much of the work normally done by the rotator cuff. By relying on the deltoid instead of the torn rotator cuff, reverse shoulder replacement may help restore shoulder movement, improve stability, and significantly reduce pain in patients who are no longer candidates for conventional anatomical replacement.

Dr Hockings performs reverse shoulder procedures using either a deltopectoral or superior approach, depending on your anatomy and clinical needs. During surgery, he also incorporates an augmented reality surgical platform called NextAR that uses smart glasses to provide live visual feedback based on your personalised anatomical plan.
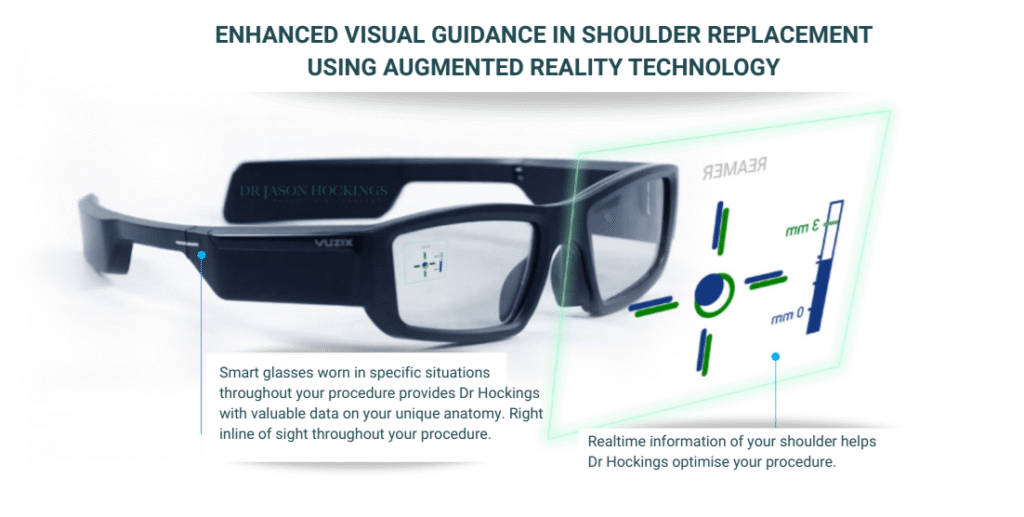
NextAR Shoulder enhances accuracy by overlaying live metrics such as:
A recent study showed exceptional alignment accuracy, with deviations from the pre-op plan as low as ~0.6° in angle and less than 1 mm in position, demonstrating superior execution of the surgical plan.
The glenosphere replaces the ball of the shoulder joint, but unlike a traditional shoulder replacement, it is fixed to the shoulder blade rather than the upper arm. It attaches securely to a metal baseplate that is anchored to the glenoid using screws. The rounded metal design creates the new “ball” of the joint and shifts the centre of rotation, allowing the deltoid muscle to raise the arm even when the rotator cuff is not functioning. Different glenosphere sizes can be selected to match the patient’s anatomy and support joint stability and mobility.

The humeral cup replaces the socket part of the joint. It is a smooth, concave liner, often made from durable polyethylene, and is designed to articulate with the metal glenosphere. The cup provides a stable surface for controlled, balanced movement and allows the deltoid muscle to power the joint. Variations in cup depth, shape, and angulation enable the surgeon to fine-tune joint tension and movement, helping to maintain stability during everyday activities such as lifting and reaching.

The humeral stem sits inside the upper arm bone and forms the foundation for the humeral cup. It is typically made from strong, biocompatible metal, and may be inserted with or without cement depending on bone quality. The stem supports the prosthesis, distributes load through the arm bone, and helps maintain alignment during shoulder movement. Different stem lengths and designs allow the implant to be matched to the patient’s anatomy, contributing to the long-term stability of the overall construct.
When the components of a reverse shoulder replacement are assembled, they work together to shift the centre of rotation, giving the deltoid muscle improved leverage to lift and control the arm. This design enhances stability when the rotator cuff is no longer functioning and allows the joint to move through a more efficient biomechanical pathway. As a result, many people can regain practical movement for everyday tasks such as reaching, lifting the arm, and dressing.
This reversed configuration is especially valuable for individuals with massive rotator cuff tears, cuff tear arthropathy, complex shoulder fractures, or previous unsuccessful shoulder surgery. Modern implant systems also provide intraoperative flexibility, meaning that if a surgeon needs to convert from an anatomic to a reverse configuration (either during the initial procedure or a future revision), certain components may be retained rather than fully replaced. This can support a smoother operation and helps preserve as much natural bone and soft tissue as possible.
This step-by-step guide outlines what to expect from your initial consultation through to surgery and recovery, using Dr Hockings’ structured and individualised approach. Every stage of your care, from pre-operative planning to rehabilitation, is tailored to your shoulder anatomy, functional needs, and recovery goals to support the safest and most effective outcome for your situation.
Step 1.

Your journey begins with a referral from your GP or another medical specialist. This referral is required to book your first appointment with Dr Jason Hockings and ensures you receive the appropriate Medicare rebate.
During your initial consultation, Dr Hockings will take a detailed history and perform a comprehensive shoulder examination to understand how your symptoms affect movement, strength, and daily activities. Imaging such as X-rays, ultrasound, or MRI may be reviewed or arranged to assess the condition of your shoulder joint, the rotator cuff, bone quality, and overall anatomy.
This appointment is also your opportunity to ask questions and gain a clear understanding of the condition affecting your shoulder. If reverse total shoulder replacement is recommended, Dr Hockings will explain why this option is suitable, outline the potential risks and benefits, and discuss the expected recovery pathway.
If you proceed with surgery, you will complete a consent form and receive guidance on preparing your home and organising any support you may need after the procedure. Additional assessments or investigations may also be arranged to ensure you are medically ready for surgery.
Step 2.

Once reverse total shoulder replacement has been recommended, Dr Jason Hockings will begin a detailed pre-operative planning process to ensure the procedure is tailored to your individual anatomy and shoulder function.
You may undergo additional X-rays, CT scans, or MRI to provide precise information about the condition of the shoulder joint, the extent of rotator cuff damage, and the shape and quality of the bone. These images help guide decisions about implant selection, component positioning, and whether any additional soft-tissue or bone procedures may be required.
During this stage, Dr Hockings will review your medical history, current medications, and any underlying health conditions that may influence your surgery or recovery. You may also be referred for routine blood tests or a pre-admission assessment to ensure you are medically prepared for the operation.
This planning phase is also a chance to discuss your goals, expected functional improvements, and any concerns you may have. Dr Hockings will outline the steps of the procedure in simple terms, explain the potential risks and limitations, and ensure you have a clear understanding of what to expect before, during, and after surgery.
Step 3.

In the weeks leading up to your surgery, Dr Jason Hockings and his team will guide you through several important steps to ensure you are well prepared. You will attend a pre-admission assessment at the hospital, where your medical history, medications, allergies, and recent test results will be reviewed by the nursing and anaesthetic team. This helps ensure your surgery is performed as safely as possible.
You may receive advice from Dr Hockings regarding:
Medications that need to be paused or adjusted before surgery
Maintaining general fitness and shoulder mobility where possible
Preparing your home environment to support early recovery (for example, keeping frequently used items within easy reach or arranging help with daily tasks)
Organising support from family or friends for the first few weeks after surgery
The hospital will provide clear fasting instructions, explain when to arrive on the day of surgery, and outline what to bring with you. If required, you may also have consultations with your anaesthetist, especially if you have other health conditions that need careful management.
Some patients benefit from prehabilitation, such as gentle exercises or physiotherapy to optimise shoulder and upper-body strength before surgery. Dr Hockings will advise you if this is appropriate for your situation.
This preparation phase helps ensure you feel informed, supported, and ready for the operation, with a clear understanding of what to expect in the days leading up to your hospital admission.
Step 4.

In the lead-up to your surgery, you will meet with an anaesthetist, either at your pre-admission appointment or on the day of your procedure. This consultation ensures you are medically prepared for anaesthesia and understand how your comfort and safety will be managed throughout the operation. The anaesthetist will review your medical history, any previous experiences with anaesthesia, your current medications, and any allergies or health conditions that may influence your anaesthetic plan. They will explain the recommended approach for your surgery, which may involve a general anaesthetic, a regional nerve block, or a combination of both, and will outline how pain will be controlled in the hours following surgery. For many patients, a nerve block is used to help support early comfort by temporarily reducing sensation around the shoulder.
You will also receive clear instructions about fasting, medication timing, and what to expect when you arrive at the hospital. This consultation is an important opportunity to ask questions and discuss any concerns, helping you feel informed and reassured ahead of your reverse shoulder replacement.
Step 5.

When you arrive at the hospital on the day of your procedure, the nursing team will guide you through the admission process, confirm your details, and ensure all pre-operative steps have been completed. You will change into hospital clothing, have your vital signs checked, and meet members of the surgical and anaesthetic teams. Dr Hockings will review your shoulder, confirm the surgical plan, and answer any final questions before you proceed to theatre.
In the operating suite, the anaesthetist will administer your anaesthetic, which is typically a general anaesthetic and may be combined with a regional nerve block to help support comfort after surgery. Once you are comfortable and fully prepared, you will be positioned safely for the operation, and the shoulder area will be cleaned and prepared in a sterile manner.
Every part of this process is designed to ensure your safety, comfort, and confidence as you move into surgery for your reverse total shoulder replacement.
Step 6.

Reverse shoulder replacement is performed under general anaesthesia, often combined with a regional nerve block to support post-operative comfort. The procedure usually takes around 1.5 to 2 hours.
Dr Hockings begins by removing the damaged joint surfaces and preparing both the glenoid and humerus with precision. The prosthetic components are then inserted in a reversed configuration, where the ball is placed on the shoulder blade and the socket is positioned on the upper arm bone. This design allows the deltoid muscle to take over the work of a deficient rotator cuff.
Dr Hockings uses advanced implant systems and digital planning tools to support accuracy and implant positioning. In most cases, the surgery is performed through a muscle-preserving approach to help protect soft tissues and support recovery.
Most patients stay in hospital for one to two nights, depending on comfort, mobility, and overall health.
Early care focuses on pain control, joint protection, and gentle movement. You can expect your arm to be supported in a sling, with the physiotherapy team guiding safe passive exercises to prevent stiffness. Pain management will be tailored to your needs using medications and, in some cases, continued nerve block support.
Weeks 0–6: Sling for support; passive physiotherapy begins
Weeks 6–12: Gradual introduction of active movement and light strengthening
3–6 months: Steady improvement in strength, comfort, and everyday function
6+ months: Return to light recreational activities; ongoing rehab for higher-demand tasks
Dr Hockings will review your progress at scheduled appointments and coordinate your rehabilitation alongside your physiotherapist. Recovery is gradual, and while experiences vary, many people notice meaningful improvements in pain and arm function over the months following surgery.
This step-by-step process is designed to deliver a personalised, precise, and thoughtful surgical experience, restoring function, comfort, and quality of life through advanced shoulder replacement care.

If you’re experiencing ongoing pain, stiffness, or reduced movement that is affecting your daily activities or quality of life, a thorough orthopaedic assessment can help determine the cause and guide the most appropriate treatment options for your situation.